Introduction
In 2022, we reported in two separate stories on the outbreak of Monkeypox virus. It is our promise at Medhealth.info to you our fans to keep you updated on health events including infectious diseases. In this publication, we will take you through a once infectious disease confined in a small part of the World but now gaining grounds into becoming a global threat. For decades, mpox was confined to West and Central Africa. However, through disease surveillance reports and epidemiological investigations, we now know that Mpox outbreak now spans multiple continents, across all six World Health Organization (WHO) regions. The zoonotic viral disease, emerged from the shadows of obscurity to become a pressing global health concern. Thus, following the May 2022 outbreak outside Africa, the disease was declared a Public Health Emergency of International Concern (PHEIC) by the WHO, meaning, countries may need to mobilize resources and enhance surveillance and the public and stakeholders are informed about necessary health measures to control the spread of the disease. In August this year mpox was again declared a PHEIC.
The symptoms of mpox mimic those of the eradicated smallpox disease, with potential for complications. The disease poses a unique threat to public health systems globally and this publication provides an exposition to why this is the case.
Historical Perspectives of mpox
The dawn of mpox began in 1958 when outbreaks occurred among monkeys kept for research in Copenhagen, Denmark. The mpox virus (MPOXV) was discovered during this outbreak, hence the original name of the disease, “monkeypox’’. Human cases of the disease did not appear until 1970 when the first human case was reported in the Democratic Republic of Congo (DRC) amidst smallpox eradication efforts. Sporadic cases were reported in Africa between 1980 and 1990. The first outbreak outside Africa was reported in the United States in 2003, linked to imported infected rodents from Africa. This outbreak raised an alarm on the potential for wider transmission. Between 2018 and 2019, an outbreak occurred in the DRC, challenging the believe that the disease was rare and self-limiting. The disease was only known for its primary transmission through contact with infected animals. While the world was still battling with Covid-19, mpox was gradually unveiling from the shadows. It was not until mid-May 2022 when a global outbreak of the disease occurred, where human-human transmission was possible among people with close physical contact, that Mpox re-emerged as a global health threat. By July 2022, the WHO declared mpox a PHEIC. Since the 2022 outbreak, Mpox continued to spread across Europe and other non-endemic regions. The WHO was prompted about the racist and stigmatizing language associated with the disease, that spread across the net and some communities. Following a series of consultations with global experts, and in alignment with the WHO’s standards for International Classification of Diseases, a new name, “Mpox” is now preferred to “monkeypox’’. On 14th August this year, the current Mpox outbreak was declared a PHEIC in alignment with the WHO’s International Health Regulations. What is unique about this outbreak? Who is at risk? Are there vaccines? We’ll find out in the subsequent paragraphs.
How mpox Develops and Its Symptoms
The pathogenesis of mpox involves the complex interaction between the virus and the human body, leading to the symptoms and complications observed in infected individuals.
The viral agent responsible for mpox is the MPOXV, a double stranded DNA virus belonging to the orthopoxvirus genus in the Poxviridae family of viruses. MPOXV enters the human body primarily through the broken skin, respiratory droplets, or mucous membranes (eyes, nose, and mouth). Its route of transmission is therefore a direct contact with an infected person, animal or contaminated surfaces. Upon entry, the virus initially infects epithelial cells (sheets of cells that give protection to the skin, mucous membranes and lines the body cavities) followed by uncoating of its covering (that is how the virus is able to insert its pathogenic structures into the infected person). The viral DNA is released and the virus replicates (produces several copies of itself) within lymph nodes, tonsils and the spleen. After replication, the virus repackages the new copies into virions (the infective form it had). These virions reinfect neighboring cells and spread through the blood stream (primary viremia) to other organs such as the lungs, the liver and gastrointestinal tract. Further replication in these organs leads to secondary viremia, which distributes the virus throughout the body. The spread of the virus to the skin is what leads to the characteristic skin lesions observed (See picture 1). In the skin this time, the virus infects epidermal cells, particularly keratinocytes. The virus replicates within the keratinocytes leading to cell lysis and inflammation. This inflammatory reaction is what causes the initial skin lesions (rashes) which begin as macules (flat, red spots). As the virus continues to replicate, immune response intensifies, fluid accumulates within the lesions forming vesicles (fluid-filled lesions). Subsequently, immune cells begin to infiltrate the inflammatory site leading to pustules (lesions filled with dead cells). Skin lesions may last 2-4 weeks. Eventually, as the immune system clears the virus, the lesions may crust over and leave scar behind due to dermal damage.
How mpox Develops and Its Symptoms
The pathogenesis of mpox involves the complex interaction between the virus and the human body, leading to the symptoms and complications observed in infected individuals.
The viral agent responsible for mpox is the MPOXV, a double stranded DNA virus belonging to the orthopoxvirus genus in the Poxviridae family of viruses. MPOXV enters the human body primarily through the broken skin, respiratory droplets, or mucous membranes (eyes, nose, and mouth). Its route of transmission is therefore a direct contact with an infected person, animal or contaminated surfaces. Upon entry, the virus initially infects epithelial cells (sheets of cells that give protection to the skin, mucous membranes and lines the body cavities) followed by uncoating of its covering (that is how the virus is able to insert its pathogenic structures into the infected person).

The viral DNA is released and the virus replicates (produces several copies of itself) within lymph nodes, tonsils and the spleen. After replication, the virus repackages the new copies into virions (the infective form it had). These virions reinfect neighboring cells and spread through the blood stream (primary viremia) to other organs such as the lungs, the liver and gastrointestinal tract. Further replication in these organs leads to secondary viremia, which distributes the virus throughout the body. The spread of the virus to the skin is what leads to the characteristic skin lesions observed (See picture 1). In the skin this time, the virus infects epidermal cells, particularly keratinocytes. The virus replicates within the keratinocytes leading to cell lysis and inflammation. This inflammatory reaction is what causes the initial skin lesions (rashes) which begin as macules (flat, red spots). As the virus continues to replicate, immune response intensifies, fluid accumulates within the lesions forming vesicles (fluid-filled lesions). Subsequently, immune cells begin to infiltrate the inflammatory site leading to pustules (lesions filled with dead cells). Skin lesions may last 2-4 weeks. Eventually, as the immune system clears the virus, the lesions may crust over and leave scar behind due to dermal damage.

While the rash develops as a result of viral replication, fever results from the release of pyrogenic inflammatory mediators that reset the hypothalamic temperature set point. Other symptoms include headache, back pain, muscle aches and swollen lymph nodes (lymphadenitis). Lymphadenitis is a unique feature of Mpox that distinguishes it from smallpox disease. See various stages of mpox scab formation in picture 2 from CDC.
Epidemiology and Geographical distribution of mpox
The epidemiology of mpox has changed drastically over time since its discovery, reflecting shift in transmission patterns, geographical distribution and populations at risk.
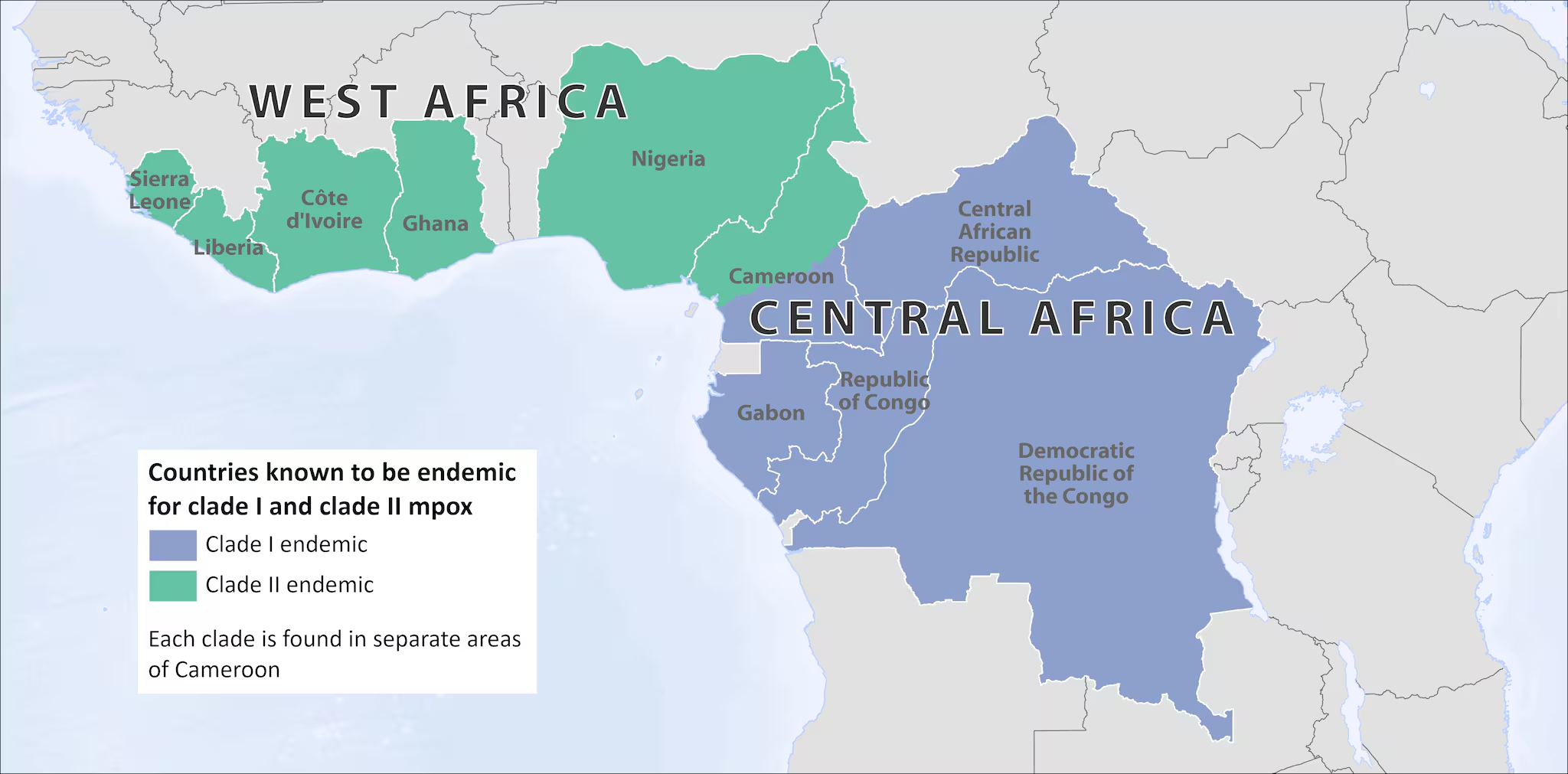
Mpox was endemic in Central and West Africa, with countries like Democratic Republic of Congo, Ghana and Nigeria reporting the highest number of cases. Twenty WHO member states in Africa have reported cases of Mpox to the organization since the beginning of January 2022. There are two main variants of the mpox virus, clade 1 and clade 2, and each has subclades. Clade 1 is believed to be more infectious and deadly than the clade 2. It includes subclades 1a and 1b and has been the cause of outbreaks in Central Africa since 2023. The subclades of Clade 2 are subclades 2a and 2b, which was the cause of the global outbreak in 2022. The clade 2b was responsible for the outbreak in the UK and was mostly spread through sex particularly among gay sexual partners. See the map here for endemicity of mpox.
As of 8th September 2024, a total of 103,898 laboratory confirmed cases, including 231 deaths have been reported to WHO. Out of this, 15 countries reported 5,759 confirmed cases, including 32 deaths. See chart for countries with highest number of cases reported.

The global mpox outbreak, which began in January 2022, reached 95,226 laboratory-confirmed cases and 185 deaths in March 2024 across 117 countries. Of those cases, 466 new cases and three deaths were reported in March alone. The African Region accounted for 39% of cases, followed by the European Region (26%) and the Americas (25%). The Democratic Republic of the Congo (DRC) continued to report the highest number of cases in Africa, with over 1,763 confirmed cases since the outbreak began. The countries reporting the largest increases in March included the Republic of Congo, the United Kingdom, Puerto Rico, and Vietnam, with notable reductions in all other regions except the Western Pacific.
Despite a 37% reduction in reported cases from February, the data likely underestimates the total burden due to underreporting and poor testing in rural regions. The global transmission of Mpox sustained at low levels, but changing levels of reporting in Africa remained a concern.
By May 2024, a total of 97,745 laboratory-confirmed cases and 203 deaths were reported across 116 countries. Africa remains the hardest hit, especially the Democratic Republic of the Congo (DRC), which accounted for 99% of the cases in the African region. A major challenge in these regions, particularly in rural areas, is the limited access to testing as stated earlier, leading to underreporting. This difficulty has highlighted the critical need for resources, as only 18% of suspected cases have been confirmed in the DRC. Other countries, such as Mexico and France, also reported notable increases in cases.
The smallpox vaccine demonstrated a strong efficacy against the MPOXV. Hence many believe that the resurgence of Mpox is partly attributable to the decline in the administration of the smallpox vaccine following improved smallpox eradication efforts in the 1970s.
Populations at risk
Mpox was historically prevalent among children under the age of 15 in endemic regions. However, epidemiological data from recent outbreaks indicates a shift towards a more adult population, predominantly males. The shift may be attributable to transmission within social groups, communities, and sexual transmission including men who have sex with men. It should be emphasized that anyone regardless of age, gender or sexual orientation is at risk of Mpox infection. Meanwhile, young children, pregnant women and immunocompromised individuals, healthcare workers and people with multiple sexual partners are at higher risk.
Treatment and Control
Treatment and management of mpox is directed at infection prevention and supportive care as per disease severity. Provided infection prevention and control measures can be maintained, the WHO recommends home isolation for mild and uncomplicated cases. Antipyretics may be given for fever, and analgesics may be given for pain, in conjunction with nutritional support and hydration. It is the recommendation of the WHO that skin lesions should be kept dry and clean to prevent secondary infection and patients should be thoroughly monitored for any complications. For complicated cases, and high-risk group individuals, hospitalization is necessary to achieve an effective symptomatic management.
In patients such as immunocompromised individuals, pregnant women and children, antivirals including Tecovirimat is recommended.
On September 13, 2024, the WHO announced a prequalified MVA-BN vaccine also known as Imvanex or Jynneos as the first vaccine to be used against Mpox. It was initially recommended for people aged 18-years and above. However, following a review by the WHO Strategic Advisory Group of Experts (SAGE) on immunization, the MVA-BN vaccine is now recommended for high-risk people under outbreak situations. The vaccine is administered as two-dose injection 4 weeks apart, with an estimated 82% efficacy in the full administration. Two other vaccines candidates such as LC-16 and ACAM2000 are under prequalification stages.
Public Disclaimer: This is meant for public information only and should not be a replacement for expert or qualified medical consult.
Authors
Solomon Awiagah & Sherrif Awiagah
Bibliography
Beeson, A. M., Haston, J., McCormick, D. W., Reynolds, M., Chatham-Stephens, K., McCollum, A. M., & Godfred-Cato, S. (2023). Mpox in Children and Adolescents: Epidemiology, Clinical Features, Diagnosis, and Management. Pediatrics, 151(2). https://doi.org/10.1542/peds.2022-060179.
Bunge, E. M., Hoet, B., Chen, L., Lienert, F., Weidenthaler, H., Baer, L. R., & Steffen, R. (2022). The changing epidemiology of human monkeypox—A potential threat? A systematic review. PLOS Neglected Tropical Diseases, 16(2), e0010141. https://doi.org/10.1371/journal.pntd.0010141.
Happi, C., Adetifa, I., Mbala, P., Njouom, R., Nakoune, E., Happi, A., Ndodo, N., Ayansola, O., Mboowa, G., Bedford, T., Neher, R. A., Roemer, C., Hodcroft, E., Tegally, H., O’Toole, Á., Rambaut, A., Pybus, O., Kraemer, M. U. G., Wilkinson, E., … de Oliveira, T. (2022). Urgent need for a non-discriminatory and non-stigmatizing nomenclature for monkeypox virus. PLOS Biology, 20(8), e3001769. https://doi.org/10.1371/journal.pbio.3001769.
Kumar, N., Acharya, A., Gendelman, H. E., & Byrareddy, S. N. (2022). The 2022 outbreak and the pathobiology of the monkeypox virus. Journal of Autoimmunity, 131, 102855. https://doi.org/10.1016/j.jaut.2022.102855.
Lu, J., Xing, H., Wang, C., Tang, M., Wu, C., Ye, F., Yin, L., Yang, Y., Tan, W., & Shen, L. (2023). Mpox (formerly monkeypox): pathogenesis, prevention and treatment. Signal Transduction and Targeted Therapy, 8(1), 458. https://doi.org/10.1038/s41392-023-01675-2.
Mitjà, O., Ogoina, D., Titanji, B. K., Galvan, C., Muyembe, J.-J., Marks, M., & Orkin, C. M. (2023). Monkeypox. The Lancet, 401(10370), 60–74. https://doi.org/10.1016/S0140-6736(22)02075-X.
Ranjan, S., Vashishth, K., Sak, K., & Tuli, H. S. (2023). The Emergence of Mpox: Epidemiology and Current Therapeutic Options. Current Pharmacology Reports, 9(3), 144–153. https://doi.org/10.1007/s40495-023-00318-y.
Simpson, K., Heymann, D., Brown, C. S., Edmunds, W. J., Elsgaard, J., Fine, P., Hochrein, H., Hoff, N. A., Green, A., Ihekweazu, C., Jones, T. C., Lule, S., Maclennan, J., McCollum, A., Mühlemann, B., Nightingale, E., Ogoina, D., Ogunleye, A., Petersen, B., … Wapling, A. (2020). Human monkeypox – After 40 years, an unintended consequence of smallpox eradication. Vaccine, 38(33), 5077–5081. https://doi.org/10.1016/j.vaccine.2020.04.062.
Van Dijck, C., Hoff, N. A., Mbala-Kingebeni, P., Low, N., Cevik, M., Rimoin, A. W., Kindrachuk, J., & Liesenborghs, L. (2023). Emergence of mpox in the post-smallpox era—a narrative review on mpox epidemiology. Clinical Microbiology and Infection, 29(12), 1487–1492. https://doi.org/10.1016/j.cmi.2023.08.008.
WHO Media Team. (2024, September 13). WHO prequalifies the first vaccine against mpox. Https://Www.Who.Int/News/Item/13-09-2024-Who-Prequalifies-the-First-Vaccine-against-Mpox.
WHO Team. (2024a, July 28). Multi-country outbreak of mpox, External situation report#34- 28 June 2024 Edition 34. Https://Www.Who.Int/Publications/m/Item/Multi-Country-Outbreak-of-Mpox–External-Situation-Report-34–28-June-2024.
WHO Team. (2024b, August 12). Multi-country outbreak of mpox, External situation report#35- 12 August 2024 Edition 35. Https://Www.Who.Int/Publications/m/Item/Multi-Country-Outbreak-of-Mpox–External-Situation-Report-35–12-August-2024.
WHO Team. (2024c, August 26). Mpox global strategic preparedness and response plan. Https://Www.Who.Int/Publications/m/Item/Mpox-Global-Strategic-Preparedness-and-Response-Plan/.
World Health Organization. (2022, July 10). Clinical management and infection prevention and control for monkeypox: Interim rapid response guidance, 10 June 2022. Https://Www.Who.Int/Publications/i/Item/WHO-MPX-Clinical-and-IPC-2022.1.
World Health Organization. (2024, August 17). Mpox. Https://Www.Who.Int/News-Room/Questions-and-Answers/Item/Mpox.
Yon, H., Shin, H., Shin, J. Il, Shin, J. U., Shin, Y. H., Lee, J., Rhee, S. Y., Koyanagi, A., Jacob, L., Smith, L., Lee, S. W., Rahmati, M., Ahmad, S., Cho, W., & Yon, D. K. (2023). Clinical manifestations of human Mpox infection: A systematic review and meta‐analysis. Reviews in Medical Virology, 33(4). https://doi.org/10.1002/rmv.2446.


Very useful ☺️
Very useful
We are glad you found this useful. Please like and share. Cheers!
Interesting
Helpful .Thanks
In my opinion, this one is one of the best articles you have written so far.
Thanks, Phenomenal!
Nice piece👏, keep on educating the general public